Diabetes Stats
Chances are you know someone with type 2 diabetes or you may be a person with diabetes yourself. The prevalence of diabetes is continually increasing. According to the American Diabetes Association (ADA), 25.8 million Americans including adults and children, have type 2 diabetes and another 79 MILLION people have pre-diabetes (most of them don’t even know it).
The Centers for Disease Control and Prevention (CDC) predicted that by 2050, up to 1 in 3 Americans will have diabetes, most having type 2. The amount of money we spend on type 2 diabetes is insanely high. According to the ADA, the total costs of diagnosed diabetes in the United States in 2012 was 245 BILLION dollars: $176 billion for direct medical costs and $69 billion in reduced productivity. Something needs to change. Before we get ahead of ourselves, let’s look at what diabetes actually is.
What is Diabetes?
There are a few different diagnosable types of diabetes, and all are related to the body’s inability to manage its glucose and insulin levels (both of which we will talk about shortly).
Type 1 diabetes (historically referred to as juvenile diabetes) is when the pancreas cannot make insulin or doesn’t make enough. Type 1 diabetes typically begins in childhood and onset is sudden. While type 1 diabetes is not reversible, it may be possible to decrease insulin dependence and pharmaceutical drugs by managing blood sugar levels nutritionally.
Type 2 diabetes is the most common type of diabetes. At one time it was called adult-onset diabetes because the diagnosis typically happened later in life. Sadly though, we are now seeing diagnoses in young children. In type 2 diabetes the pancreas produces insulin, but the body becomes desensitized to its effects. Type 2 diabetes develops gradually over time and for the majority of people it is both preventable and reversible.
Gestational diabetes develops during pregnancy and often disappears after the baby is born. However, high blood sugar levels often lead to high birth weight infants, childhood obesity, and increased risk for type 2 diabetes in the child. Women who experience diabetes while pregnant have a greater chance of reoccurring gestational diabetes in subsequent pregnancies and developing type 2 diabetes later in life.
Normal Blood Sugar Response. You might remember from previous posts that the key players in the blood sugar response are carbohydrates, glucose, and insulin. Here’s how it works:
1. Carbohydrates, regardless of the source (bread, pasta, rice, vegetables, fruits, cookies, candy, soda) turn into sugar in the bloodstream (glucose).
2. Glucose in the bloodstream stimulates the production of insulin by the pancreas.
3. Insulin allows glucose entrance into the cells for use as energy and drives blood sugar levels down to normal. This only works if cells respond to insulin.
Insulin Resistance. If the cells are exposed to too much sugar, too much insulin, and too often because blood sugar levels are constantly elevated (from eating too many carbs or too much sugar), they become desensitized. Insulin resistance occurs when the cells become resistant to the blood sugar lowering effects of insulin. This develops over time, as a result of eating too much sugar or processed carbohydrates on a regular basis for many years. It’s like when you walk into a noisy party and can’t hear a word your spouse is saying, and after a little while, you can because you begin to drown the noise out. That’s what happens with insulin resistance as your cells are bathed in insulin and no longer “hear” the insulin’s command to open the door to your cells to take in the glucose, thus lowering blood sugar levels. The good news is that by balancing our meals and snacks to reduce our sugar and processed carbohydrate intake, we can prevent or reverse the damage in our cells!
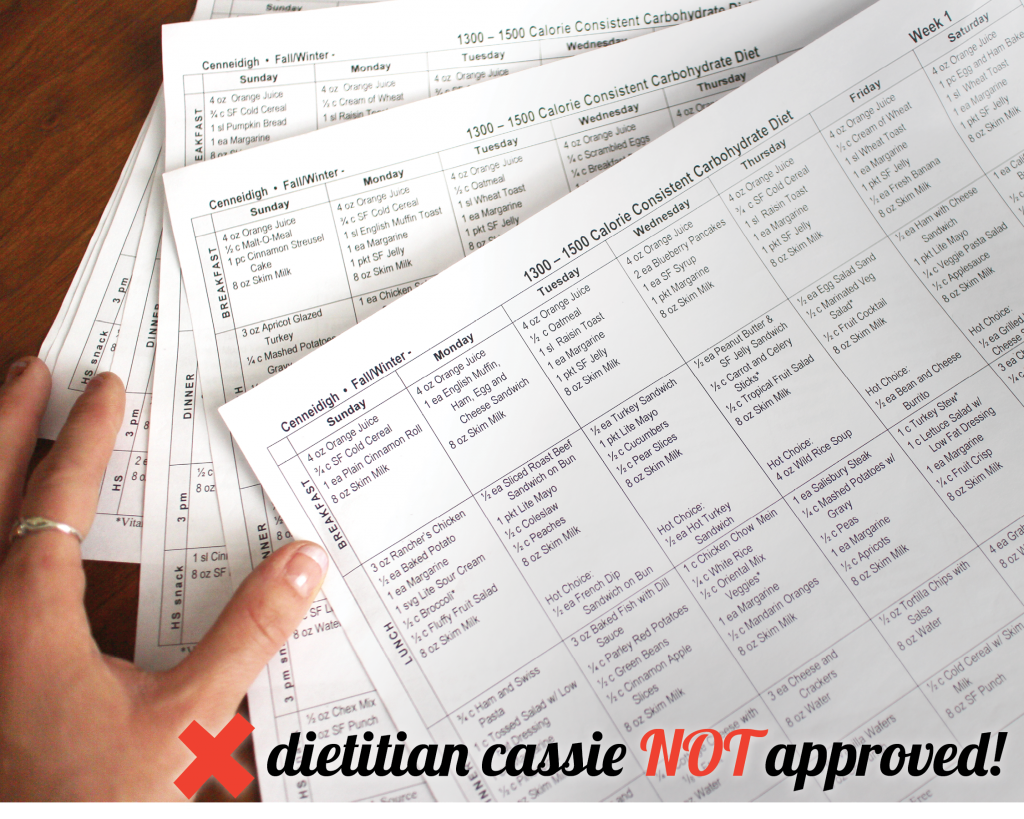
Conventional Treatment. The standard diabetes treatment approach targets elevated blood glucose levels with medication, and for the most part, overlooks the power of nutrition to address the root cause of diabetes. I believe this is a backwards “after the fact” approach because it focuses on treating the symptoms rather than the underlying cause. When it comes to nutrition for diabetes, carbohydrate counting is the gold standard. Carbohydrate counting is ensuring that diabetics are getting “enough” carbohydrates for blood sugar control, with the general goal being 45-60 grams at meals and 15-30 at snacks. Reminder: carbohydrates are the VERY thing that cause spikes in blood sugar levels. In the words of one of our clients: “Why are so many carbs recommended in diabetic diets? So they can prescribe us more insulin?” Your guess is as good as mine, friends. Mainstream foods recommended for diabetics include egg whites, oatmeal, sugar-free Jello, whole wheat crackers, rice, pasta, beans, skim milk and diet soda (see meal plans shown below that were created for a diabetic client by a dietitian and check out the video at the end of this post where a doctor and dietitian debate about the best way for diabetics to eat). I believe that coincidentally, the low-fat, high-carbohydrate way of eating that has been widely promoted as the ideal diet for weight loss and disease prevention is largely responsible for fueling our current diabetes epidemic.
Get my Sugar Craving FREE Guide!
There’s a Better Way.
We teach our clients to eat the same whether they have diabetes or they don’t want to get diabetes. The bottom line is blood sugar regulation. Get off the blood sugar roller coaster by eating balanced with less carbs and ample amounts of protein and healthy fat. Fats don’t raise blood sugars, carbohydrates do. Healthy fats are important for everyone, especially for people with diabetes and they have nothing to do with blood sugar or insulin. They help slow the digestion and absorption of carbohydrates, helping our blood sugar levels stay stable instead of spiking and dropping (which happens when we don’t include fats). Eating PFC balanced by including protein and fat along with carbohydrates is an excellent way to keep blood sugar levels stable and reduce the need for insulin.
6 Tips for keeping blood sugars balanced:
1. Put the brakes on sugar. A great first step is removing the foods that spike blood sugar levels most. Instead of putting prescription drugs into the body to mitigate the consequences of eating too much sugar, reduce the amount of sugar you’re putting in in the first place! (What about artificial sweeteners? Even though artificial sweeteners like Splenda are often recommended by doctors, dietitians and diabetes counselors, they may still affect your blood sugar levels since your [super smart] body anticipates the glucose after tasting the sweetness on the tongue and may secrete insulin to manage perceived incoming sugar load. For more info on artificial sweeteners, check out this post.)
2. Choose the best carbs. Not all carbohydrates are created equal! Processed carbs like cake, cookies and soda turn in to a lot more sugar than fresh veggies. You can read more about the types of carbohydrates in this post. Many people forget that vegetables and fruits are carbohydrates too, not just the bread, pasta and grains! Whether they’re whole or not, grains are still refined and processed, and refined, processed foods will never be better for us than real foods. Choose fruits and veggies for your carbs as often as you can — they’re the only carb sources we need to be healthy.
3. Don’t completely eliminate carbs. Eat some carbs. When embracing the balanced PFC approach, it can be tempting to omit carbs completely. I mean, if carbs turn to sugar and sugar leads to all sorts of health issues, why include them at all? I believe for most people the body runs best when it gets a balance of all 3 macronutrients: protein fat AND carbs! Everyone’s biochemistry is different so our serving sizes might be different, but it’s important to be sure we’re including enough healthy carbs along with our protein and healthy fat to really THRIVE and live life to the FULLEST. Carbs are not the enemy, it’s eating them on their own or indulging in too MUCH of them that can become a problem.
4. Eat plenty of healthy fat. We know that healthy fat is important for everyone, for a million different reasons, and especially for people with diabetes. If I were to pick one population who especially need to eat fat, even more than most, it would be people with diabetes or blood sugar issues. It’s easy to consume fewer carbs when you pair ‘em with fat because of the wonderful fat satiety factor: it fills you up! Fat is the best buffer for carbohydrates, and it lowers your insulin requirement. I recommend at least a couple tablespoons of healthy fat at every meal and snack from avocados, butter, coconut oil, olive oil, nuts, seeds, cheese, olives, coconut milk (the canned kind), heavy cream and coconut cream.
5. Supplement for optimal support. We recommend targeted quantities of these nutrients in the form of supplementing with high quality pharmaceutical grade formulas that can only be sold through a licensed practitioner (the kind we offer in our Real Food Vitamins Store). Our top three supplements that we recommend for all of our clients with diabetes or pre-diabetes, are Metabolic Synergy, GlucoVive™, Berberine Synergy, and it can also be very beneficial to use a blood sugar balancing protein powder and the basic gut health supplements (Glutamine, Fish Oil and a Probiotic). Our clients see great results when adding in these key supplements in addition to focusing on eating PFC balanced.
6. Be proactive. You can test your own blood sugar levels at home with a glucometer and interpret your results to know your risk of diabetes. To learn more about this, check out our virtual coaching program with one of our Dietitian Coaches.You don’t need to do this alone. We can help you manage your blood sugar levels with real food. It’s always exciting to see clients come OFF their meds as they change their lifestyle! ☺
To sum it all up: The key to preventing, managing or even reversing type 2 diabetes is to eat the kinds of foods that help keep your blood sugars stable. Eating lots of carbs means potential for insulin resistance. Balanced PFC eating = eating fat and protein with less carbs = reduced need for insulin = balanced blood sugars for a healthy, happy life!
Grab the guide below for my BEST tips to BUST (and prevent!) sugar cravings so that you can gain control of your blood sugars and get to your healthiest self and more energetic life!











Great post Cassie!! Good food is so powerful!!
Good stuff Cassie. So glad you are able to be one of our awesome presenters at the Reversing Diabetes World Summit! You certainly know your stuff!!
Hi and thanks for listening to my presentation through the Reversing Diabetes World Summit. That is such a great question, Margo! Blood sugar responses are so individualized and can sometimes react differently than we’d expect them to. For those with diabetes the blood sugar increase in the morning is often times referred to as the “Dawn Phenomenon.” In our coaching sessions, myself and my other health coaches help our clients find an individualized eating regimen that helps to balance their blood sugar levels and support their health and goals. If you’d like our help in helping you navigate this PFC way of eating, please let us know by emailing [email protected] for details 🙂
My husband was able to get off of insulin and glipizides by completely eliminating carbohydrates for almost two years. Now, he realized that this extreme diet was not healthy to maintain, but he got off all the diabetic meds, and dropped 75 pounds during that time. He then started to slowly add carbohydrates back into his diet, carefully checking his blood levels to ensure he wasn’t going back into a diabetic state. He would probably be considered low carbohydrate at this point. He still avoids fruits and vegetables (except for an occasional potato or green chile), but has added back flour and corn tortillas, beans, and an occasional loaf of bread. All of those are homemade, so he can control exactly what is in them. He looks great, and has lots of energy. Best of all, he never has to worry about going into hypoglycemia from the drugs.nNow, as a caveat, not everyone has a metabolism that allows this to happen. He has a sister who is getting off of her diabetic meds using this approach, but has not lost any weight. Also, my husband had been on the glipizides for about 15 years, before being put on insulin. He just suddenly decided he was not going to give himself shots in tummy fat three times a day. He carefully reduced his meds over about four months time, to avoid shocks to his system, and that caused several episodes of hypoglycemia that scared all of us (we kept a stash of tootsie rolls for those times). By staying on the protein-fat diet for so long, his body reset, but it was not easy. He is very happy to be back on carbs, even extremely moderate carbs.
Thanks for sharing!!
Oh my. That video was so painful to watch! No wonder some people scoff at the profession of dietetics. I’m a future RD (start my internship in January) and I’m so glad to have someone like you around!
Hi! Do you have much experience with gestational diabetes? I’m 29 weeks pregnant and have been trying to manage it with my diet but have been having very frustrating results this past week. I have been gluten free for a year and eat primarily a whole food diet (I try – I’ve cut out almost all highly processed foods and continue to do so where possible), but I’m not perfect – pregnant with 3 young children at home. I try to incorporate traditional foods made with bone broth into my diet several times a week, fermented foods such as kefir, kombucha, sauerkraut, etc., no refined sugar and very limited raw honey or maple syrup (usually only on weekends – honey with my coffee and a small amount of syrup with breakfast, but not every weekend), protein from the best sources, and healthy fats. I am overweight, I came into this pregnancy overweight trying to heal from issues with hypothyroidism and a lifetime of eating poorly. I had GD with pregnancy #2, but not #1 or #3. My doctor gave me a meter to check my blood sugar at home and my fasting levels have been around 100, give or take a few points. I live overseas, and occasionally shop at the military base, so when we went last week I had a moment of weakness and bought some chips that I know I shouldn’t have eaten – they were loaded with MSG and food dyes, etc. The next day I could tell that my blood sugar was off. I was falling asleep all day long, and did some random post meal checks and my blood sugar was higher than it had ever been (150s, 2 hours after eating). When I went to my doctor the next day, he said I needed to monitor my blood sugar 4x/day for 2 weeks and then go back and see him (he said he wanted to put me on glyburide, but I think insulin is a safer bet). Since then, I’ve been diligent about writing down my food and have been trying to follow a more ‘diabetic’ diet – counting carbs at meals and trying to eat every few hours. At lunch and dinner I’ll get 1-2 servings of carbs from grains. The rest of my carbs throughout the day, which are limited (but not limited enough, as I’m reading) are coming from fruit, kefir, kombucha, etc. Anyway, the past 2 mornings I’ve woken up and my fasting blood sugar has been even higher. 128 yesterday and 132 this morning! This is after cutting out a lot of carbs and adding in more vegetables throughout the day. I usually only have 1 serving of fruit a day, in the afternoon or after dinner. I’m very frustrated because I don’t really know where to turn for advice. Since I’m overseas I don’t have a choice in doctors. The dietician at the hospital (I haven’t met with her, but got this info from my doctor) ascribes to the old FDA food pyramid and advises way too many carbs. The doctor is middle of the road, he says I should cut whatever she says in half. But I’m really frustrated because when I do cut carbs my blood sugar skyrockets. I know they’re the problem and that I have insulin resistance, I just don’t know what to do. I know I could exercise more and plan to incorporate that, but I’m confused at why, when instead of serving a starch at a meal, I serve an extra vegetable, I end up with higher blood sugar levels.
Hi Janis!
We sure do have experience helping clients manage gestational diabetes and hypothyroidism too. I’m sorry to hear how frustrated you are—would love to help you with this! We find that it’s more than just eating real, whole foods/following a gluten free lifestyle, but the combination of macronutrients (P, F and C) is critical, and differs based on individuality. Please email us at [email protected] for our help— we can get you in as soon as this next week (and we have appointments in office and via phone or Skype)!
Hi Laura! There is a huge connection between adrenal fatigue and diabetes. Cortisol (known as your “stress hormone”) is released in response to stress, anxiety and lack of sleep. Cortisol raises blood sugar levels, which cause your pancreas to release insulin to bring the excess sugar to your cells to be stored as fat. It’s important to get adrenal fatigue under control to keep blood sugar levels stable and reduce the need for insulin. My team and I would love to help you navigate what would be best for you— just shoot us an email info at healthysimplelife.com 🙂